Before I discuss Stem Cell Therapy, it’s important to discuss the history of this so-called fountain of youth. Stem cells were discovered before I was born some 60 years ago. I was in graduate school at Penn State University in the 1980s, when our scientists isolated stem cells in adipose (fat) tissue. Prior to that, stem cells had already been discovered in umbilical cord blood. While in medical school at University of Temple School of Medicine, the first umbilical cord stem cell transplant was used to treat blood dyscrasia in 1988. Mesenchymal Stem Cells (MSCs) we’re officially named by Dr. Arnold Caplan from Case Western Reserve University over 26 years ago. Since that time, there have been hundreds of clinical trials and stem cell clinics, many who are claiming medical benefits to treat a variety of diseases including multiple sclerosis (MS), amyotrophic lateral sclerosis (ALS), acute spinal cord injuries, and other orthopedic disorders, including osteoarthritis (OA). Some of the early clinical results appear very favorable, however, level one clinical studies are lacking.
Because the term “Stem Cells” have been used by patients to infer that these cells will differentiate into regenerating tissue producing cells, Dr. Caplan has renamed them “Mesenchymal Signaling Cells” to more accurately reflect their mechanism of action. These Mesenchymal Signaling Cells do not differentiate into cells but they most likely signal the patient’s own resident dormant stem cells to activate. These active resident stem cells are thought to construct new tissue at the site of injury.
What Are Stem Cells and Why Are They One Of The Most Searched Medical Terms On The Internet?
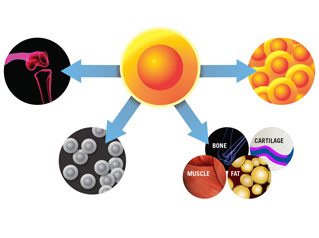 Stem cells are living, undifferentiated cells that have the capabilities to self-replicating in culture and differentiate into cartilage, fat or bone (multipotent). They are found in every organ in the human body. They keep us healthy by augmenting the natural healing process in our body by modulating our inflammatory and immune system. Therefore, they have the potential to repair and regenerate damaged or diseased tissue. Many believe they do this by decreasing inflammation and scar formation, while promoting increased blood supply to the injured area.
Stem cells are living, undifferentiated cells that have the capabilities to self-replicating in culture and differentiate into cartilage, fat or bone (multipotent). They are found in every organ in the human body. They keep us healthy by augmenting the natural healing process in our body by modulating our inflammatory and immune system. Therefore, they have the potential to repair and regenerate damaged or diseased tissue. Many believe they do this by decreasing inflammation and scar formation, while promoting increased blood supply to the injured area.
I was once asked by a patient this simple question: “If our stem cells are so great, why do we get sick?” The answer: sometimes our stem cells stop working, malfunction, or wear out. It is important to know that there are different types of stem cells and to understand what their advantages and disadvantages are.
There are three different types of stem cells:
1. Embryonic stem cells
2. Autologous adult stem cells
3. Allogenic post-natal stem cells
Embryonic stem cells are pluripotent and therefore able to form any tissue type. However, they have a high potential to form tumors and they raise ethical issues. We do not work with embryonic stem cells.
Autologous adult stem cells come from our own bodies. These cells are present in our bone marrow and body fat. They are referred to as Bone Marrow Aspirate Concentration (BMAC) and Adipose Derived Stem Cells. These cells can be harvested through a minimally invasive procedure and be minimally manipulated prior to being injected back into the patient in the same sitting.
Allogenic post-natal stem cells are harvested from the umbilical cord and amniotic products of live healthy births. Each stem cell type has advantages and disadvantages, but its notable that these allogenic products can be very useful in patients older than 60, where there are concerns about the quantity and potency of their own stem cells. A small volume of allogenic stem cells can contain millions of cells. In addition, there is no harvest morbidity. Treatment involves a painless ultrasound procedure.
I recently developed problems with my knee that prevented me from performing everyday activities as well as exercise. Despite conservative therapy, my symptoms continued. An MRI of my knee showed significant pathology; most surgeons would have recommended surgical intervention after failing to improve with months of conservative therapy. With my work and family schedule, surgery was not a good option for me. I had benefitted from regenerative therapy on the same knee 15 years prior, so I felt confident it would work again. Therefore, I decided to receive an injection of post-natal Wharton’s jelly stem cells into my left knee.
(At 60 years old, I was concerned that my own bone marrow or adipose tissue may not have enough stem cells to resolve the cartilage issue in my knee, but if I were younger, I would have seriously considered using my own stem cells from either my bone or fat.)
Two weeks after my injection I was back on my mountain bike. I recently played beach volleyball with no issues—an activity that I haven’t dared to challenge since I played college football. I am absolutely amazed at the continued improvements since.
The misconception, with both autologous and allogenic stem cells, are that they differentiate and turn themselves into new tissues inside the body. While it’s not perfectly clear how they work, it is more likely that these cells stimulate our own autologous stem cells to replicate, repair and regenerate our tissues. Even Dr. Caplan has since called to rename MSCs to Medicinal Signaling Cells, to more accurately reflect their true function of signaling our resident stem cells by secreting bioactive factors. It is our own site-specific and tissue-specific stem cells that ultimately do all the work.
Autologous BMAC (treatment using one’s own stem cells) has been approved by the Food and Drug Administration (FDA) to treat various disorders, however, the cell number and variability has a tendency to decrease as we age. Adipose-derived stem cells from our fatty tissue has the same advantages and disadvantages as bone marrow—both require a surgical harvest, and their volume decreases with age. Recently, the FDA issued a warning about only using minimal manipulation of the cells once removed from our body. This may eventually limit the number of techniques currently being used to isolate adipose derived stem cells.
Both autologous and allogenic stem cells are believed to offer both short-term and long-term benefits as they respond to inflammatory signals from injured tissues. This process appears to occur by modulating our inflammatory and immune processes. These cells have the capability to secrete hundreds of growth factors, cytokines, exosomes and micro RNA that secrete anti-inflammatory and auto immune modulators that help fight inflammation and even prevent the breakdown of collagen, the substance that gives our tissue structure and integrity. Some of these compounds act directly at the site of injury, while others act indirectly by modulating our immunologic response and increasing blood supply to the injured area.
There are many things we can do to optimize the anti-inflammatory, autoimmune and angiogenic (formation of new blood vessels) effects of these stem cells and their byproducts—and the most important may be optimizing the environment in which they work. It is not uncommon for us to see a discouraged patient who tried a form of stem cell therapy somewhere else and failed to improve. Most of the time, these patients were given treatments or products that actually contained no stem cells. These treatments neglect the principle of optimizing the environment in order to optimize stem cell function. Some of these patients should have never been talked into an expensive, experimental treatment, and others should have had an attempt at correcting underlying issues that contributed to their poor result prior to stem cell therapy. There are many things we can do to optimize results prior to undergoing Regenerative Therapy.
The most important factor is to first determine if you are a good candidate for this type of treatment, because not everyone is. The next step would be to find out how you can optimize your results, or possibly become a viable candidate.
At the Athletic Institute of Medicine, it is our goal to help determine if regenerative medicine techniques are right for you, and to optimize your chances of successful treatment. Please review The Seven Questions You Need to Ask Your Provider Prior to Considering Stem Cell Therapy.